Introduction
eSwatini (formerly Swaziland), a small population-sized sub-Sahara African country characterized by its highest human immunodeficiency virus (HIV) prevalence globally. It has 86% of its people living with HIV on antiretroviral therapy (ART) (
1,
2). From 2010, the Government of eSwatini has demonstrated a high level of commitment to virally suppress in HIV spread among the population. Of those living with HIV and on treatment, 94% are virally suppressed (
3). eSwatini's dual testing and treatment programs of tuberculosis (TB) and HIV have been successful (
4). eSwatini's life expectancy is estimated at 58 years (
5).
From 2013 to 2019 prevention of mother-to-child transmission (PMTCT) Option B+ program was being rolled out by M’edecins Sans Froniesres (MSF) and the eSwatini Ministry of Health. With a 40% HIV/AIDS prevalence rate among pregnant mothers, if not treated, 25% to 40% of the children born from HIV-positive pregnant mothers are not spared from infection (
6). The eSwatini 2014 PMTCT statistics showed a 1% increase of HIV-infected babies born and infants aged 6 to 8 weeks (
7). In 2015 deliveries were estimated at 34 571, therefore ensuring that HIV+ pregnant women receive PMTCT services was critical to reducing HIV+ women transmitting the virus to their children (
6,
7). It is important to note that in 2017 WHO reported that eSwatini's 10 400 pregnant women living with HIV received antiretroviral for PTMCT, 95% of pregnant women with HIV who received ART for PTMCT, 78% of infants born to women living with HIV receiving a virological test with 2 months of birth (EID), and final mother-to-child transmission rate including breastfeeding period (
4,
5). This was good progress toward making a generation free of HIV.
UNICEF and the eSwatini Ministry of Health have been improving the training of mentor mothers, health workers from the 11 healthcare facilities that offer maternity services to increase integrated community support for retention in care (
8). By 2019, a total of 150 000 HIV-exposed children were uninfected, 1800 new HIV infections averted due to PMTCT, 10 433 pregnant women received antiretroviral (ARV) for PMTCT achieving a +95% coverage of pregnant women receiving ARV for PMTCT (
3). Nevertheless, HIV is still the country's biggest public health concern as witnessed through the need of ARV for PMTCT by pregnant 9900, unavailability of data on HIV testing among pregnant women, and early infant diagnosis (
3). Functional public healthcare institutions, skilled community healthcare workers, and health education are critical to the success of PMTCT Option B+ intervention, yet little is known regarding HIV+ pregnant mothers’ lifestyle and experiences. The purpose of this study was to explore, describe perceptions and experiences of HIV-positive pregnant women regarding the PMTCT, Option B+ program.
Methods
Research design: The study used qualitative, exploratory, and descriptive research design. This paradigm necessitates an understanding of social situation, event, role, or interaction and in this case of exploring and describing the perceptions of HIV+ pregnant mothers regarding PMTCT Option B. This study was conducted in a semi-urban setting, in one Public Health Unit of Manzini Region, a pilot site of the PMTCT Option B+ program in the country. The facility caters for out-patients and offers preventive services and public health programs. Services offered include provider-initiated HIV testing and counseling (PIHTC), PMTCT, ART, antenatal care (ANC), child welfare services (CWF), sexual transmission infection (STI) treatment, and laboratory services, among other services.
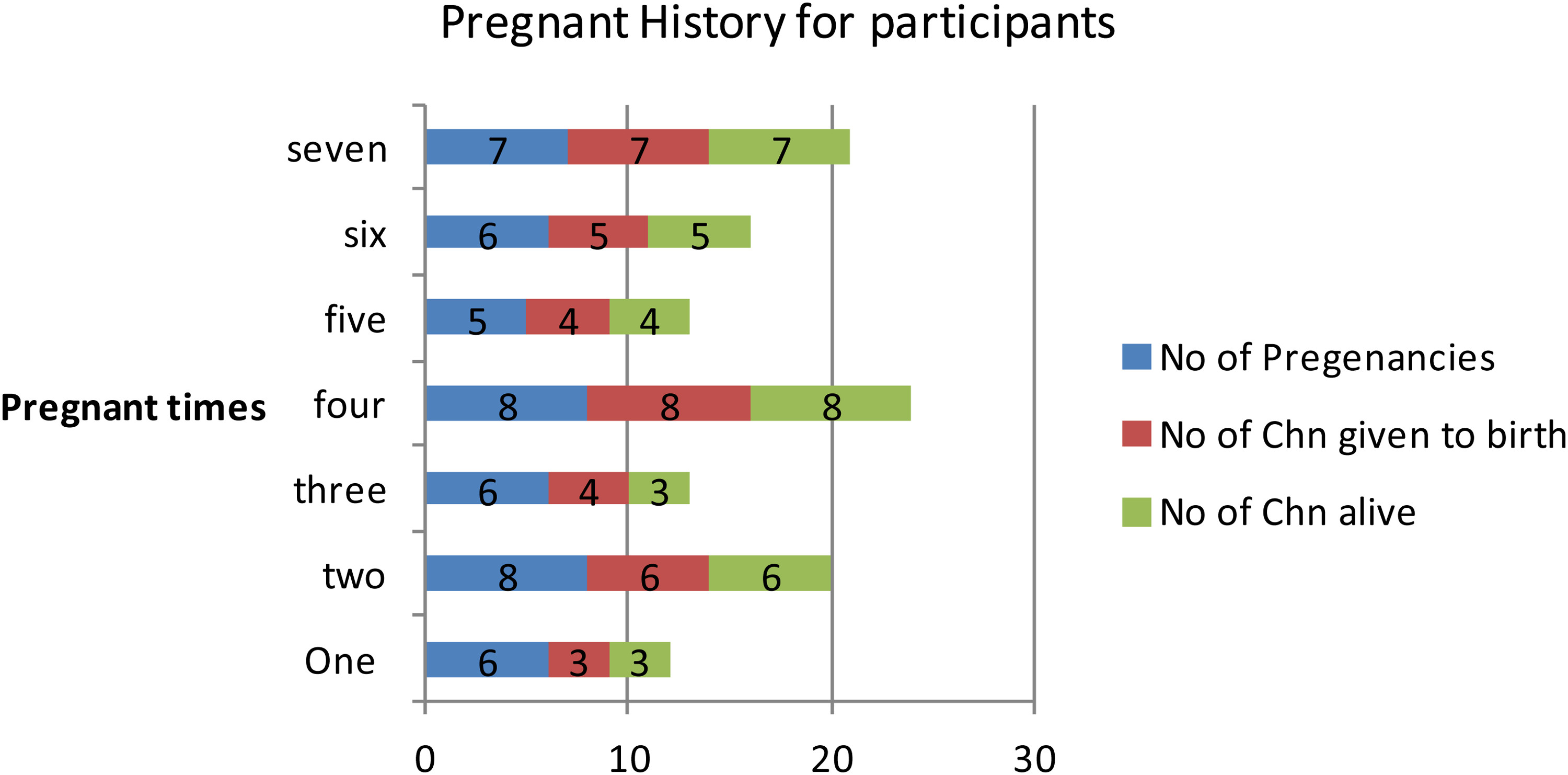
Sample: Twenty HIV-positive pregnant mothers who had were enrolled on the PMTCT Option B+ program at a Public Health Unit in the Manzini region of eSwatini. Thirteen were in the first trimester, 5 in the second trimester, and 2 in the last trimester, respectively. Informed consent was obtained from participants and was written in English and translated in siSwati Subjects were briefed that they were recorded during interviews and their recordings were only used for research academic purposes. Only 17 mothers consented and assented and voluntarily signed the consent form. Refusal to participate in the study had no effect in any way on healthcare services where they receive their care.
Inclusion Criteria
The selection criterion for the study was that participants had to be:
•
HIV-positive pregnant mothers speaking siSwati language at least between the ages of 18 and 40 years.
•
Enrolled in the PMTCT Option B+ program during the current pregnancy.
•
Attending antenatal care service in a Public Health Unit in Manzini, the study site, willing to participate voluntarily.
Exclusion
•
Pregnant mothers not enrolled in the PMTCT Option B+ program during the current pregnancy.
•
Unwilling to participate, pregnant mothers, although enrolled in the PMTCT Option B+ program.
Ethical considerations (see Ethical Approval)
Data Collection
In-depth semi-structured interviews were conducted on one-to-one for a period of 1 month. Review of the interview guide was done by the Health Research Ethics Committee, nurse manager, and nurses working at the Public Health Clinic involved in providing the PMTCT Option B+ program services. A pilot study to check the validity and reliability of the interviews was done and Cronbach's α =0.78. All interviews were recorded using a tape recorder after obtaining permission from the participants. All healthcare workers at the public health care center were notified prior to the session so that nobody enters the interview room disturbing the interview progress. Considering the subject's privacy to sensitive issues, a private quiet interviewing room was labeled “INTERVIEWS IN PROGRESS DO NOT DISTURB” on the door. Each interview record was labeled with an assigned code according to the date and time the interview was conducted. The interview periods ranged between 30 and 40 min per participant. An experienced and knowledgeable research assistant was incorporated for taking field notes during the interviews.
Data Analysis
Data were analyzed using the following step-wise format. Descriptive wording for the topics was assigned as abbreviated and identifiable codes connected to data segments. These topics were actively constructed into themes derived from data sets, categorized, and coded in alphabetized format for easy interpretation. Thematic analysis is an appropriate method for seeking to understand respondents’ experiences, thoughts, and behaviors across data set that answered our research questions. The themes were: perceptions of respondents on being enrolled in the PMTCT Option B+ program, understanding about PMTCT Option B+ program and information needed with regard to PMTCT Option B+ program, perceptions with the care received from the nurses, and their assistance on PMTCT Option B+ program, Effectiveness of the PMTCT Option B+ program and Challenges of taking ARVs (see Appendix). All related data were computerized and preliminary qualitative analysis was done. This was followed by interpreting and reporting the research findings.
Discussion
eSwatini has swiftly moved towards mother-to-child transmission (PMTCT) Option B+ intervention which encourages all HIV+ pregnant and breastfeeding mothers to instigate a life time antiretroviral therapy despite CD4+ count level. Functional public health care institutions, skilled community healthcare workers, and health education are critical to the success of PMTCT Option B+ intervention, and knowledge regarding HIV+ pregnant mothers’ perceptions and experiences is essential.
Participants perceived enrolling on the PMTCT Option B+ program, as preventing mother-to-child-transmission of HIV. Antiretroviral therapy is well-known as a life-saving intervention in HIV infection. It helps to boost the immune system, CD4 count and prevent opportunistic infections that they may develop. For successful immune restoration and preserving the structural integrity of lymphoid tissues, engaging in early ART can prevent AIDS-associated events, restricting cell subset imbalances and dysfunction. The findings were in support of World Health Organization that one of the benefits of ARV prophylaxis for PMTCT is to increase maternal life expectancy (
6,
9,
10). The participants understood that Option B+ could help them live a better and a longer life enabling them to raise their children for a much longer time before they die (
11). It is known that HIV can be transmitted from an HIV-infected positive woman to her child during pregnancy, childbirth, and breastfeeding. Antiretroviral treatment and other effective PMTCT interventions can reduce the risk to below 5% (
12). PMTCT Option B+ program provides antiretroviral treatment to stop their infants from acquiring the virus. Most studies that evaluated the benefits of Option B+ program focused mainly on clinical benefits through early initiation of lifelong antiretroviral therapy (
10,
11). PMTCT, Option B+ requires initiation of all HIV positive pregnant and breastfeeding women onto lifelong antiretroviral therapy (ART), regardless on CD4+ cell count or WHO clinical staging and for infants, a daily nevirapine (NVP) or zidovudine (AZT) from birth through the age of 4-6 weeks regardless of feeding method (
13).
The HIV-positive pregnant women displayed a good knowledge and understanding of the PMTCT program. The participants stated that they took one tablet at a time, once every day, and for it to be effective they do not mix with some traditional herbs. Many herbs and supplements contain undeclared pharmaceutical drugs, heavy metals, and other contaminants, and practices such as mixing low doses of ARV drugs into herbal remedies would harm patients by leading to the development of viral resistance (
14). Participants displayed good understanding of the fact that life-long ART is initiated immediately regardless of CD4 count and patients should start ART immediately when they are diagnosed with HIV. Once one started taking the ARVs one was expected to continue for the rest of your life. Our findings indicated that the nurse-midwives in the facility provided both verbal and written health information to the HIV-positive pregnant mothers. The information included; attending all clinical appointments, adherence to treatment for Option B+, retention improvement strategies, infant post-natal follow up, ART side effects and what to do if their medication runs out before the due date. Findings showed that good nutrition has a greater impact at the early stages of HIV, strengthening the immune system to fight opportunistic infections (OIs) and delaying the progression of the disease. Similar findings were observed that good nutrition can play an important role in the care and management of HIV (
15). However, challenges were noted on those HIV-positive pregnant mothers with an unstable source of income and who cannot afford a proper diet.
Although the participants experienced good nurse-patient care at the public health care facility, disclosure of their HIV-positive status to their husbands and families was one of the main challenges. HIV disclosure status was significantly predicted in many low- and middle-income countries (
16,
17,
18). Our findings show that some of their partners if they know their HIV+ status they even leave them. This might be related to the stigma associated with HIV, fear of negative consequences from their friends, partners, and perception to preserve family stability (
19,
20). Some women indicated that they needed assistance on the side effects of the ART drugs and what they can do if they run out of their medication before the due date. HIV-positive women needed proper counseling on the advantages of adherence to the drugs and disclosure during drug provision. This was supported by findings in the study about the level of adherence and predictors of adherence to the Option B+ PMTCT program in Tigray, Northern Ethiopia (
21). The healthcare workers provided education and counseling regarding ART side effects. Further explanation was given regarding on some instances where immune restoration may be erratic causing acute inflammatory responses mostly during ART initiation. The immune reconstruction inflammatory syndrome and /or incomplete with residual inflammation despite being on antiretroviral therapy may lead to non-infectious morbidity and mortality despite that the mortality rate is slim compared to HIV+ infected people not on ART.
eSwatini healthcare professionals and UNICEF have recognized that persistent HIV-related stigma is a huge obstacle to more effective HIV responses under Option B+ program. Fear of disclosure, one consequence of HIV-related stigma is common among all people living with HIV, including pregnant women (
19). Healthcare clinical and community workers in along with UNICEF to close the gaps between women and men are reducing stigma by directing addressing social, cultural, and legal contexts that perpetuate HIV-related stigma. To reduce the gaps between gender HIV-related stigma healthcare workers at pilot sites had to consider for individual and couple counseling appointments before and after initiating ART and educate men about HIV and ART.
Pregnant women believed that the PMTCT Option B+ program was very effective as it prolonged life span especially for those who adhere to treatment and take ART drugs every day and at the same time. Others added that the intervention was very effective as it protects the baby from being infected during pregnancy, delivery, and breastfeeding. The outcomes of having an HIV-negative baby can motivate HIV-positive pregnant women to adhere to the treatment and accept the program. This was in contrast with a previous study about perceptions of pregnant women on the PMTCT of HIV program at the antenatal care unit and maternity ward at the Jordan Heynes community (
22). Under Option B+ intervention, all the HIV-infected pregnant mothers have an advantage of ART simplification, protection against MTCT in future pregnancies, continual prevention against sexual transmission to serodiscordant partners (
20). Indeed, avoiding “stop-start-stop” increases longevity among HIV-infected populations (
23).
Limitations
This study has a number of limitations. The study was conducted on a single Public Health Unit and findings were generalized to represent the region. The eligibility criteria were only was only HIV+ pregnant mothers who initiated ART during pregnancy, thereby ignoring those who initiated ART prior to pregnancy. Sampled women were living in semi-urban settings who may not reflect experiences of HIV+ pregnant mothers from most of the country rural settings.
Strengths
Few studies have explored the experiences of HIV+ pregnant mothers on PMTCT Option B+ intervention; hence it gives critical insights among this group. HIV-positive pregnant women’s concerns should be addressed especially the side effects of ART drugs. Gaps in psychological care and support were identified. Rampant HIV tests among men and women need to be done in both urban and rural areas. To our knowledge, this study is the first to explore patient experiences on Option B+.